Cancerous Prostate
On Friday 22 Nov 2019, I had my prostate removed (Radical robot-assisted prostatectomy) at the Sydney Adventist Hospital (the San). A recent biopsy showed a Gleason score of 8 (out of a possible 12). A very aggressive cancer. Scans show that it had not spread to lymph or bones – to where prostate cancer likes to migrate. However, the biopsy showed that it had got out of the top of the prostate. I will know more in a few weeks when a follow up PSA will tell us how much cancer remains.
I’m writing this 7 days after the op. At home. With a catheter – which will be in place for another 4 days. After the catheter is removed, I can expect to be incontinent until I can learn to use my pelvic floor muscle again. I am not allowed to lift anything heavier that a 2 litre milk bottle for at least 6 weeks. I am allowed to walk.
In radical prostatectomy, the prostate and surrounding tissue is removed. (It came out through my umbilicus.) Unfortunately, the urethra carries its urine through the prostate on its way to the penis. That is now gone, so the operation involves stitching the hole bringing urine out of the bladder directly to the hole at the back of the penis – one oval the other round. The catheter has to stay in place to give that junction a chance to bind. No pelvic floor exercises until the catheter is removed.
It is often said that ‘most men will die with a prostate cancer but not of a prostate cancer’. I might be one of the ones ‘who dies of a prostate cancer’.
OK. A bit of history. Back sometime in the early 1990s, my GP Bob Sebesfi put his finger up my bum and announced that I had an ‘enlarged prostate’, sent me for tests and put me on medication. Over the years, that medication changed to FlowMaxtra and then to Duodart. I had PSA tests every 6 months or so which showed a steady decline in the PSA (due to the medication). All trotting along nicely.
Then, earlier this year, I had a recall from my now GP Peter English who noticed a kick up in the PSA value (up from 2 to 4.5). Because of the action of Duodart, that 4.5 is equivalent to 9 – a high reading). I was sent of to a local Urologist. I chose to see James Symons who is part of the Riverina Urology practice (as well as a couple of Sydney practices). I then had a series of scans and tests and then a biopsy. Three weeks after the biopsy (which identified the Gleason score 8 cancer) I was on the operating table in Sydney. Very quick. Not quicker because time had to pass following the biopsy to reduce inflammation and ensure minimal infection from the biopsy.
We flew to Sydney on Thursday the afternoon before the op and Helen stayed at Jacaranda Lodge in the grounds of the Adventist Hospital as accommodation for use of Regional patients. Only a few metres from the building in which I was a patient.
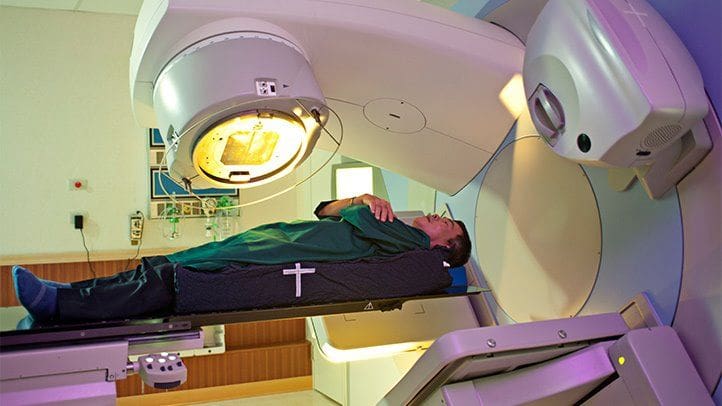
The operation was robotic assisted which means there is no major external wound. I have 6 holes across my belly where ‘robotic arms’ were inserted and manipulated by surgeon James Symons. Use of the robot was why I had to fly to Sydney. Wagga does not have that equipment.
The operation took 6 hours. A bit longer than normal because of an abnormal bone spur somewhere. I was completely zonked out for the rest of the day with the remains of the anesthetic. Even on Saturday, I was fairly ordinary and they had to bring in a physio to get me walking. He set me the task of walking around the ward at least 2 times and if possible 4 times the following day. I was a bit jolted that they had to bring someone in to get me to walk. I did just over 50 laps around that ward on the Sunday. With my rapid improvement, surgeon James said I could be discharged that day – Sunday. I chose to wait another night and was discharged before 10 am on Monday 25 November – three days after the surgery. Unfortunately, I slept very little on Sunday night.
When we had walked the 200 metres to Jacaranda Lodge, I took one look at the room and realised I would not be comfortable sitting in the chair or lying on the bed. We booked a flight back to Wagga at 3pm that afternoon. Helen furiously packed and my friend Bruce McLennan came to drive us to the airport. Our neighbour Bernie Conway picked us up from Wagga the airport and drove us back home. By the time we got home, we were both exhausted. Not enough sleep.
This was a major operation, even if I don’t have a big wound to remind me. I am trying my best to live as normal a life as I can within the constraints of catheter and exercise. I did manage to get to my violin strings lesson on Wednesday (I could not concentrate well enough to play well.) I went to the social walking group on Thursday and walked a kilometer. Today, my skin was having a reaction to the dressing covering the hole from where the surgical drain was removed on Sunday. So, we went into the Riverina Urology rooms where their nurse removed all the dressings. Tonight, I walked 1.5km around our village. Things are going well.
The 7 holes across my belly now make me more susceptible to hernia. Hence the very strong warning of ‘no lifting’ for 6 weeks. On removal of the catheter next Tuesday, I will be incontinent while I learn to use that pelvic floor muscle. We’ve been provided with a small supply of incontinence pads. I have appointments booked with a physio to help with those exercises.
As well as getting fit and mobile again, my next major step will be the first post-op PSA which will show how much of the cancer remains. Further treatment will depend on that result.
An update a few days later. On Tuesday 3 Dec, after a cystogram to test for leaks, I had the catheter removed. Surprisingly painless. Then began the dreaded incontinence pad regime. I am to measure the percentage of what I drink ends up in the pads. The first day was a lot 15%. The next day just 1%. Yesterday, after a lot of activity and a Xmas party 1.5%. Today (6 Dec) will be less than 0.5%. No drama.
I am really appreciative of many people in this journey.
- Helen’s support is extremely good. I am clearly a person who needs to be independent and Helen is navigating that obstreperousness with skill.
- James Symons for his speed of action and ability and to communicate. I am so impressed at the effort he puts in for my care and his ability to explain and answer my questions and concerns.
- The nursing staff at the San were extraordinary. Especially Kathleen and Michelle. Dedicated to assisting people when they are helpless.
- Sue Burt for teaching all those enjoyable exercises classes to help with the pelvic floor.
- Bob Sebesfi for putting his finger up my bum and getting me on a path of treatment.
- Peter English for acting promptly to an elevated PSA result.